Mitch Altman via Flickr
Corona and Public Health Policy in Germany

Benjamin Ewert
Fulda University of Applied Science
Benjamin Ewert is a Professor of Health Policies and Health Professions at the Fulda University of Applied Science in Germany. His research focuses on behavioral insights, co-production, and social innovation in the realm of health policy. He is co-editor of the book Behavioral Policies for Health Promotion and Disease Prevention (Palgrave Pivot, 2019) and has published articles in academic outlets such as Public Administration, Public Policy & Administration and Policy & Politics.

Kathrin Loer
University of Applied Sciences Osnabrück
Kathrin Loer is a Professor of Political Studies at University of Applied Sciences Osnabrück in Germany. Her research focuses on consumer science and consumer policy, public health, energy policy, behavioral policy, policy research, advocacy/lobbying, and civil society organizations. She is co-spokesperson of the Advisory Board for Consumer Research of the Federal Ministry for the Environment, Nature Conservation, Nuclear Safety, and Consumer Protection. She is an expert on policy instruments in health and consumer policy as well as behavioral public policy. Her research also focuses on expert involvement and the role of scientific evidence in policy making. She is co-editor of the book Behavioral Policies for Health Promotion and Disease Prevention (Palgrave Pivot, 2019) and has published several articles in academic outlets such as the Journal of Comparative Policy Analysis, Public Health and Policy & Politics.
Kathrin Loer was an NRW Fellow at AICGS from October until December 2019.
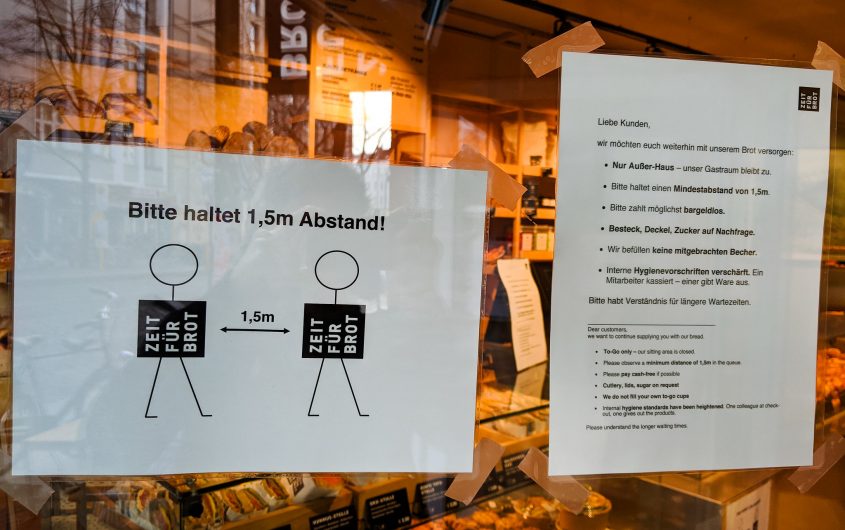
“It’s COVID-19, stupid!” In Germany, we saw a quick turnaround in responses to the spread of the virus. As the German population has learned about the importance of prevention policies, it has also had to learn how to cope with the upper end of the scale of “strict” prevention measures that intervene considerably with our personal lives. Until very recently, such strict behavioral prevention was unimaginable in Germany, relying as it does on exit restrictions, contact bans, and the observance of a minimum distance in public space. These massive restrictions on individual freedom are politically highly unattractive. Chancellor Angela Merkel felt compelled to explain to citizens that the “corona measures” were “not recommendations but rules.” After all, a high level of state attention and restrictive interventions do not really fit in with the basic principles of German prevention and health promotion policy. Traditionally, the latter has had a comparatively weak and subordinate role. Even the “Prevention Act,” a federal law aimed at increasing the significance of prevention and health promotion that was painstakingly introduced in 2015 after years of dispute between the responsible actors, changed little about this.
Before the corona virus, the rather half-hearted efforts of politicians to maintain and improve people’s health were mainly characterized by voluntary offers to “join in.” In practice, prevention policy meant low-key state commitment and friendly encouragement—public campaigns or small financial contributions toward, for example, individual training against back pain. Not only have systematic strategies regarding the health of the population as a whole been lacking up to now, but there have also been no intentions to increase the state’s responsibility in key areas of prevention. This is now abruptly changing due to the corona epidemic: measures for prevention and health promotion are firmly at the top of the political agenda. Even if this does change again (which is highly likely) when the threat of the corona epidemic vanishes, we assume that prevention policies will become much more visible in the future and take on a new significance—an opportunity for all areas of prevention and health promotion.
Public Health and Prevention in Germany: Marginalized, Complex, Politically Risky
The timidity of German prevention policy has many causes. We see three main reasons why prevention and health promotion, as part of health policy in Germany, are only marginally or not at all present. First, prevention policy, and above all a policy on “public health,” has problematic connotations from the Nazi era. Second, prevention in federally-governed Germany is an institutionally complex policy field, for which the federal states (Länder) in particular (but not only) are responsible. This complexity is currently evident in the difficulties in coordinating corona measures appropriately between the federal government and the Länder. Complexity starts when it comes to specific rules for schools and higher education. School and universities should follow a general idea of protective measures advocated by the German government, but this needs to be organized by the Länder. Some Länder allow their universities to hold classes of up to twenty students, others are not even allowed to administer exams even with social distancing rules. Complexity can also be found in the economic and service sector, e.g., with regard to the types of stores that are allowed to open or services that can be offered.
Furthermore, there is a high degree of complexity seeing the broad spectrum of actors involved in general: Actors in the statutory health insurance system (SHI) are responsible for the implementation of prevention measures. At the same time, the public authorities of the Public Health Service (ÖGD), including, among others, the Robert Koch Institute (RKI), the Paul Ehrlich Institute, the Federal Center for Health Education (BzGA), as well as state and local health authorities are responsible in different spheres. Third, prevention and health promotion has proved to be a highly unattractive and more often than not very controversial topic for politicians because taking preventive action requires intervention, more or less, in individual lifestyles. Just think of the heated debates of the past: the laws to protect non-smokers or the measles protection law from 2020. Public outrage was immense even for proposals with a much lower threshold, such as the idea to introduce a “Veggie Day” in school cafeterias. To put it plainly: The political commitment to prevention and health promotion has, so far, been anything but politically profitable. All in all, the reasons mentioned above lead to a “soft” and not very coherent prevention policy, or are typically campaigns such as “IN FORM,” a federal initiative for healthy food and more exercise, instead of measures and individual responsibility instead of solidarity and responsibility for society as a whole—without any systematic state strategy.
The political commitment to prevention and health promotion has, so far, been anything but politically profitable.
Before the corona crisis, the priority setting and slow pace of German prevention policy was a cause for great surprise: Figures for non-communicable diseases (NCDs) such as obesity, diabetes, and cardiovascular and respiratory diseases have been rising significantly for years. Currently, NCDs are estimated to account for 91 percent of all deaths in Germany. Policymakers have so far countered this worrying development with behavioral prevention instruments, i.e., a mixture of information, educational offers, and appeals (if they counter it at all). Even though the “Prevention Act” explicitly identifies living environments such as kindergartens, schools, workplaces, and homes for the elderly as places where people’s health is to be protected and promoted, genuine health prevention is hard to be found. Effective prevention would require designing living conditions that compensate for social inequality and would require building up infrastructure to overcome structural disparities and design a healthier environment for all people, e.g., in connection with social policy measures. Furthermore, it would call for action to extend cycle paths in cities or to decide in favor of stricter requirements on pre-packaged food, the amount of sugar and salt in food, etc. However, all these policies are considered politically risky, as such measures collide heavily with economic interests of producers, who earn more money by selling unhealthy food and beverages. Measures to prevent infection remain not only disparate with regard to the different federal states, but also mostly timid. We observed disparities especially in the case of vaccination policies, which the Länder have always developed differently in their public health strategies, reaching from almost binding standards to very loose measures to inform people. So far, this timidity has been explained by the fact that all interventions of prevention policy touch on a social value that is in conflict with the idea of prevention: the freedom of the individual.
Corona as a Pathbreaker?
Does the corona epidemic change this perspective? Does the virus have the effect of a “catalyzing event”? Can it bring about a change in German prevention policy? The current case shows tendencies in this direction. On the one hand, this concerns the choice of instruments. As an urgent and threatening health hazard, Corona seems to have legitimized a strong state that forces its citizens to change their behavior instead of politely inviting them to do so. According to a survey by Infratest dimap in early April, 93 percent of those people questioned supported the restrictive corona measures taken by the federal government. However, the resolute intrusion of politicians into the population through “hard rules” (Chancellor Merkel), as Germany experienced from March to May, is not a blueprint for future prevention policy. Nevertheless, it is clear that (temporary) restrictions and bans, the necessity of which are plausibly explained, are no longer a political no-go. The extremely high social value of health seems to justify such an approach and even shows its priority over economic and financial policy interests in times of the corona epidemic. In this context, it is interesting to note that a communication strategy that has become rather out of fashion in crisis-free times has also proved to be beneficial: the appeal to social solidarity and public responsibility in the sense of preserving the smooth functioning of state institutions. And even more so, it is in the interest of all to keep the health care system “alive” and working, and to protect at-risk groups and medical and nursing staff. Can this shift in perspective be maintained in the future? Since the beginning of May we have seen how a comprehensive system of intrusive policies shifts to a colorful map of different approaches in Germany’s sixteen Länder. There is a cluster of Länder (e.g., Bavaria, Baden-Wuerttemberg and Lower Saxony) that not only established quite strict rules comparatively early, but also have followed those rules for a longer time. We also find a cluster of Länder (e.g., Saxony-Anhalt, Saxony, Mecklenburg-Western Pomerania) that applied less intrusive rules. State governments supported and promoted different approaches especially when it came to re-start economic procedures, rules for schools, care facilities, and the service sector (especially restaurants and food service). One notable example is Thuringia minister-president Bodo Ramelow’s decision to depart from the rule to forcing people to use face masks.
At the same time and more generally, the corona crisis painfully illustrates how extremely relevant the second pillar of prevention policy is: situation or context-based prevention that considers social and environmental circumstances. It is the constitutionally founded duty of the state to procure sufficient protective equipment, intensive care beds, and ventilators before they are needed. Not only is the continuous renewal of pandemic plans obligatory, but also the development of new strategies that ensure greater state responsibility and control in the provision of care. The Bundeswehr, for example, could play a new role and build a strategic alliance with the Technisches Hilfswerk (THW), a federal agency within the Federal Ministry of the Interior. It is a task force providing humanitarian and technical help in any kind of crisis. Such an alliance of Bundeswehr and THW would have to be comprehensively equipped in an up-to-date standard to adopt medically relevant tasks, including research and development for vaccines.
The crisis is also changing the institutional mode of prevention policy. Although the Federal Minister of Health, Jens Spahn, is a central figure in the “Corona Cabinet,” he is nevertheless highly dependent on the support of his colleagues at the federal, state and local levels. Their support not only depends on current COVID-19-developments that differ across states and regions, but it is also very much dominated by political interests of leading economic actors and other stakeholders within their constituency, by specific developments on regional and local levels, and, of course, by specific conceptual and normative ideas of parties they belong to. Furthermore, containment of the virus is not possible without cooperation across policy fields, also known in Public Health as “Health in All Policies.” At least in the first weeks of the outbreak of the epidemic, health was the common goal of all departments. This could also apply to the fight against so-called lifestyle-related, non-communicable diseases, for which a complex spectrum of factors is responsible.
Unexpected Paths? Chances for Future Public Health Policies in Germany
Above all, it is important to what scientific expertise guides the executive decisions being made. The interaction between science and politics is currently undergoing an unprecedented stress test. In particular, the growing impression that the country is (at least indirectly) governed by virologists is fatal for at least two reasons: first, because, as the head of the Department of Virology at the Berlin Charité, Christian Drosten, emphasizes, “scientists are not politicians” and they therefore bear no political responsibility; second, because the expertise of other scientific disciplines must be equally relevant to the decision-making process for the design of effective prevention measures. For example, from a virologic point of view, initial restrictions may be just what is needed, but from a social-psychological point of view they can be counterproductive, as they increasingly demoralize people or even evoke medically unreasonable behavior. The warning of the German Ethics Council that it must be possible to question the corona measures underlines that the combination of a (too) strong executive and trust in the judgement of a supposedly leading science (in this case virology) is highly problematic. The consequence is, as Daniel Cohn-Bendit recently commented in a newspaper interview, “a restriction of democratic political leeway for society.”
What are the long-term learning effects of the epidemic for state prevention policy?
What are the long-term learning effects of the epidemic for state prevention policy? We see four essential aspects: First, the crisis experience, which is existential for many people, should lead to a fundamental upgrading of prevention and health promotion in politics. Both must no longer take place in health policy niches, but must become the central goal of politics. Primary attention must be paid to health prevention that takes social inequalities and social determinants into account. Structural precautions protect the population as a whole and relieve the individual from disproportionate personal responsibility. Closely related to this is the second idea: The question relevant to overcoming all health crises must be discussed broadly and openly: How deeply can the “preventive state” penetrate individual life, intervene in every day routines, and limit individual rights and freedom? Third, public health service at the local level must be revitalized and expanded throughout Germany, as health scientists have repeatedly called for. Health authorities, whose staff know the local health conditions and regularly check and positively influence conditions, are predestined for effective community-based prevention work. Strengthening this work also has a preventive effect on democratic politics: prudent, citizen-oriented, and, above all, local health authorities make executive intervention in the name of health unnecessary in the event of a crisis and thus, prevent the acceptance of collateral damage to society. And fourth, the ability of state infrastructures to act must be fundamentally reviewed: Are the health care system, research, civil defense, state institutions, and the Bundeswehr suitably equipped and integrated in a targeted manner so that they can act well and effectively in the event of a pandemic? Reforms are likely to be indispensable in all the areas mentioned above, from which, in our view, new opportunities and fields of action may emerge. All this requires courageous and swift political decisions.








